Xavier was moved to the Progressive NICU on Thursday night. When we left him that afternoon, he was doing great. He was still breathing fine with nothing new to report. We talked to the on call dr since Xavier's dr was visiting Harris' NICU for the day, and he told us repeatedly how impressed he was with Xavier. He smiled and told us, "This little guy thinks he's older than what he is."
When Tim called his nurse later that night to check on him, she told him that he had been moved to the PNICU since he was doing so well! This is definitely a step forward, which is what I pray for each and every day, all day. Babies are moved to the Progressive Unit once they are considered not critical.
Visiting him yesterday in this unit was a whole new ball game. The room is noticeably brighter. There are open cribs in the whole room instead of walls and walls of incubators with tiny spaces for parents to squeeze in next to them. There aren't as many monitors and machines wailing and beeping constantly. Toys, rocking chairs, car seats, and swings are in the room. Moms can be seen holding the babies and breastfeeding. There are also volunteers that visit this unit to hold the babies and cuddle with them. This makes me feel better since it is impossible for us to be with him all day, and the nurses do not have time to hold babies just to cuddle. The unit is just much more relaxed. This will be his new home until he is released, which I am hoping will be within the next 4 weeks.
Saturday, May 28, 2011
Thursday, May 26, 2011
Growing
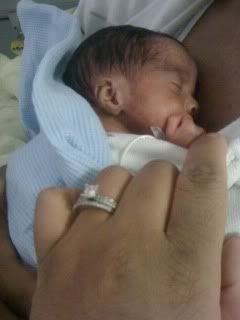

It is hard to tell from pictures just how small Xavier really is. When people see his picture, they immediately exclaim that he looks like a big boy, or that he doesn't look like he's only 2 1/2 lbs. Seeing him in person is an entirely different experience.
Yesterday, I decided to take home one of the diapers he wears for comparison to a newborn diaper sample that I have.


He is getting bigger every day, and each day we see him he looks like a new baby. He has more hair now, his skin is getting darker, and his features are becoming more defined. I try not to get caught up in his weight since we are in for a long journey. I decided instead of asking each and every day how much he weighs, I will ask his nurses once a week how much he weighs. This is how they are charting his progress anyway since daily weights tend to fluctuate.
Wednesday, May 25, 2011
No More CPAP!
Instead of doing 3 hours off and 3 hours on to give Xavier's nose a rest, his doctor decided that he no longer had to use the CPAP at all! He has been machine free for about two days now. Usually babies go from being on a vent, to the CPAP, to a nasal canula, but Xavier has avoided both the vent and canula to breathing 100% unassisted! I am so very, very happy and thankful for that. I knew he could do it because there have been so many occasions when he had removed it on his own and was breathing just fine. I am so thankful for his nurse Raye :-) for pushing his doctor to give him a chance to try it on his own. She believed in him and knew he could do it!
His dr wants me to try breastfeeding him next week. Hmmm. Not sure how that's going to go since his mouth is the size of a dime and my breast is.....much larger than that. This will definitely be interesting.
His dr wants me to try breastfeeding him next week. Hmmm. Not sure how that's going to go since his mouth is the size of a dime and my breast is.....much larger than that. This will definitely be interesting.
Monday, May 23, 2011
Break from CPAP

Today when I went to see Xavier, I immediately noticed that he had removed his CPAP. It was resting on top of his nose instead of inside of his nose. He HATES his CPAP. His nurses say that he moves so much that he pushes the little prongs further in his nose than it needs to go. This is one of many occasions that he has removed it somehow. The nurse practitioner decided that since he was doing so well breathing on his own and breathing room air from day one, she would try him off of the CPAP for three hours. So what will happen now is that he will do three hours off the CPAP and three hours on. This will give his nose a rest. The prongs are uncomfortable for him and push his nose flat against his face, piggy style. I held him today kangaroo style and his breathing remained stable the entire time. He didn't desat once, and his oxygen levels stayed 97-100. If he does well on and off the CPAP, they will start to wean him off of it early. His nurses are impressed. They usually don't wean them off until they are closer to 32 weeks. Nearly all the nurses on his floor came to see this little peanut free of his machines so soon.

Today was my first time seeing him free of all the machines. The cpap has kind of molded his nose flatter against his face than is natural, but he's so beautiful, and of course the creases will resolve itself once he's able to give his nose a rest!
Sunday, May 22, 2011
Holding Xavier

Two days ago, I was finally able to hold Xavier. He was "no-stim" for the first three days of life, which meant that he couldn't be touched except when necessary. I was so nervous as the nurses handed me his little body. He is so small and fragile that it was hard to believe that I was holding anything. I held him and rocked him for close to an hour, but I could have held him forever. When the nurses came to put him back in the incubator, she discovered that his CPAP had been accidentally disconnected. She was shocked that his breathing and heart rate stayed the same, even though he wasn't receiving any air pressure from the CPAP. He is not ready to come off of the CPAP, but it is still amazing that such a little guy could hold his own for so long without it. I'm looking forward to the day when he graduates from it.
Yesterday, I held him skin to skin as part of kangaroo care. The nurses placed him inside of my shirt, and he curled his little body against me as if he were still in the womb.

I would give anything to give him another 6 weeks, but sharing this tender moment with him was a wonderful feeling.
Friday, May 20, 2011
Xavier Grant

May 16, 2011, I woke up just after 12 am with slight pains in my side and lower stomach. Baby was moving and seemed very unsettled. I sleepily rubbed my stomach, and tried to go back to sleep. I dozed off for a few minutes, then was awaken by the same pains in my side and lower stomach. I waited for it to pass, then tried to go back to sleep. The pains didn’t subside. It was then that I noticed that the pains were coming in a pattern. I turned on my cell phone and began to time the pains, looking for a clear pattern. Five minutes apart. This was much more serious than pain; these were contractions. I had been there before, and the night seemed eerily similar to the day I gave birth to Layla. Tim was at work, I woke up in pain, and something inside of me was telling me it was show time.
I jumped out of bed, and received confirmation that I was indeed in labor. I had diarrhea and a little bit of spotting. Oh no, I thought, not again. I ran a quick bath and called Tim to come home to sit with Layla while I went to labor and delivery. I began to pray and plead to the universe that this was false labor and that our baby boy would not be born so soon. I pleaded for another month, week, or even just one more day for my son to stay with me. I drove to the hospital repeating the same prayer over and over, only pausing to call Dr. Westerholm to tell her I was on my way to labor and delivery.
The drive to the hospital was agonizing for me. I didn’t have the pain of a typical woman in labor. Instead of physical pain, I felt pain in my heart for what was almost certain to come. I could feel our son kicking so low, almost as if he were already in the birth canal. I willed my body to hold on to him.
I finally arrived at the emergency room, and was whisked away to labor and delivery by an E.R. nurse. She wished me luck and left me with the labor and delivery nurses in the prenatal observation room. Minute by minute, my anxiety built. The nurses could not find baby’s heartbeat with the fetal monitor or Doppler. I could feel him move, so I knew he was fine, but I also knew not being able to find his heartbeat was not a good sign. The nurses tried to reassure me that this sometimes happens with babies that gestational age. I wanted to point out that I had had no problem finding his heartbeat since I was 9 weeks pregnant, but I couldn’t speak.
Dr. Westerholm returned my call while I was lying on the observation table and told me that since I had had intercourse recently, all of the drama was probably due to false contractions. I wanted to believe that, but my soul was telling me otherwise. She gave authorization for the nurses to check my cervix, and I was immediately given the news that I would be delivering shortly. The nurse removed her gloved hand from my body and it was covered in blood. She told me that I was dilated to 6-7 centimeters, she felt a bulging bag of water, and she had felt him kick her hand. My heart dropped. The nurse reclined the table all the way back and told me I was to remain flat and still until the doctor came to deliver me. My heart was heavy as I called and told Tim the news.
The anesthesiologist made it to my bedside first. He explained the process of receiving a spinal for a cesarean section, but the explanation fell on deaf ears. I could barely hear more than my heartbeat at the point, and nothing else mattered. I kept going over the statistics in my head that I have googled so many times before. I began to calculate the likelihood that my baby would survive. All I wanted was for him to live.
Dr. Westerholm arrived, and seeing her face at my bedside spoke volumes about the seriousness of delivering so early. She apologized over and over. She was heartbroken because she was on our side throughout this pregnancy. She wanted this baby to be term just as much as we did. I want you to understand that this time may be a little different than last time. Layla Bug did so well, but this baby is five weeks earlier. A baby is viable at 24 weeks, and the risk of mortality decreases each week then drops way off around 28 weeks, which is about where we are today. I heard the unspoken words clearly.
She did an ultrasound to verify presentation and told me that I would be having a cesarean. Baby was still transverse, so a vaginal delivery would not be possible. What was more was that I would be having a classic cesarean because of baby’s position. Your uterus will forever be weakened and you will never be able to deliver vaginally in the future.
I was numb as I was prepped for surgery. The anesthesiologist attempted to administer my spinal while I was lying down in an attempt to prevent my bag of waters from rupturing, which could lead to baby falling into the birth canal. He tried twice unsuccessfully. The team sat me up for the spinal, and in this position it was completed in one attempt in less than 15 seconds. I was later told that I was sitting in a pool of blood. I was too numb to notice. I felt the anesthesia take hold of my body as the team helped me to recline flat on my back. I looked into the surgical lights and could see my body reflected in the glass of the light bulbs. It was an out of body experience to see my body lying there but to not be able to feel it.
Surgery began and Tim was escorted to my bedside. We stared into each other’s eyes and did not need to speak. We both saw the shock, hurt, fear, and disappointment of being faced with another preterm delivery. Our fingers laced together as the journey began. The anesthesiologist’s voice was a dark cloud above my head as he explained that the delivery room would probably be silent when baby was born. You may not hear crying. If you do hear crying it will be very brief while baby is intubated. The breathing tube that will be inserted blocks the vocal cords… I floated away to wait for my son.
I felt tugging and pressure.“Delivery!” a nurse announced the arrival of Xavier Grant. I heard a gurgle and cries filled the room. All three doctors and nurses expressed surprise that he was breathing and crying! Tears rolled down my cheeks, and I thanked God for that small miracle. I tried to catch a glimpse of the piece of my soul that would forever live outside of my body, but the team of NICU nurses blocked my view. Apgar numbers were announced at 8 and 9.
I waited patiently to see my son. The NICU team finally brought him to see me, and I was completely humbled at the sight of him. I stared at his little face and listened to him cry. He was so small and fragile, yet his presence was so powerful. He no longer belonged to just me; I would have to share him with the perils of the world and all things unknown. Life had just begun for Xavier, and as he was taken to the NICU, I made the promise that many in my position have made before me: I would dedicate my life to making his better.
Subscribe to:
Posts (Atom)




